What can be done to reduce the risk of developing more skin cancer if they have already had basal or squamous cell skin cancer?
Melanoma in Fort Washington, PA
ABOUT MELANOMA
While melanoma is seen less frequently than other kinds of skin cancer, it’s considered one of the most concerning forms of skin cancer. It can be a very aggressive skin cancer and can be fatal if it is not addressed early enough. A yearly skin cancer screening can aid in the early detection and prevention of this cancer, and it is crucial if you have a personal or family history of melanoma. With annual screenings at the Dermatology and Skin Cancer Institute, board-certified dermatologist Dr. David Kasper and Dermatology Certified Physician Assistants Amy Hahn, PA-C, Charlie Capaci, PA-C, and Megan Quinn, PA-C can monitor your skin for abnormal or evolving moles and ensure your skin is healthy. Typically, melanomas show up as a new mole or as an existing mole that grows, changes shape, changes color, begins to itch, etc. Any moles that change color to very dark or black, grow, have blurred or uneven borders, bleed, or itch are potential melanomas.
Melanomas form when the pigmented cells in the epidermis, called melanocytes, become malignant. This is most usually due to the skin cells being damaged by UV exposure, either from the sun or tanning beds. This type of damage happens at the DNA level, which causes the cells to mutate or multiply very rapidly, which creates the visible abnormal growth. Patients can also be genetically vulnerable to developing melanoma, and these individuals are particularly at risk for DNA damage from sun exposure. It is vital to get annual skin cancer screenings — or bi-annual if you or a family member have had skin cancer before. It’s also very important to learn to perform regular mole checks and self-examinations. Contact the Dermatology and Skin Cancer Institute today to schedule a skin cancer screening so you can learn more about skin cancer prevention and detection.
CAUSES
Virtually anyone can develop melanomas, particularly those with a history of sun or UV exposure or those genetically predisposed. Individuals with a primary relative, for example, a sibling, child, or parent, have a higher potential for developing a melanoma. Other risk factors include:
- Having a high number of moles or having large-sized moles
- Having light-colored or red hair
- Having blue, green, or gray eyes
- A history of tanning bed use (even if you never burned)
- A history or sun exposure (even if you never burned)
- A history of multiple or severe sunburns
SYMPTOMS
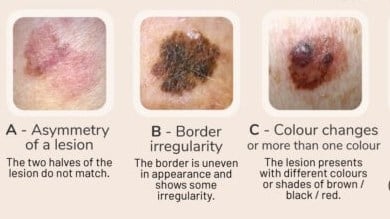
At the Dermatology and Skin Cancer Institute, we use the ABCDE method to help you understand how to spot any potential melanomas on your skin:
- A: Asymmetrical (malignant moles usually have one side that is bigger or differently shaped than the other)
- B: Borders (malignant moles usually have irregular or blurred borders)
- C: Color (malignant moles are typically dark in color or are multi-colored)
- D: Diameter (a diameter of more than 6mm, or about the size or a pencil eraser, is a sign of malignancy)
- E: Evolving (moles that grow or change in any way should be checked right away)
Harmless freckles and moles can also have some of these factors, so it’s best to have a full-body skin examination so all of your moles can be checked by a board-certified dermatologist.
MELANOMA TREATMENTS & PREVENTION
At the Dermatology and Skin Cancer Institute, Dr. Aradhna Saxena typically removes melanomas via the standard of care surgical excision.
This involves removing the cancer with a scalpel, along with a margin of normal-appearing surrounding tissue, and then stitching the surgical wound. This surgical excision is performed with a local anesthetic and is an outpatient treatment all performed in one day.
For greater margin control necessary in some cases, Dr. Aradhna Saxena will recommend a staged excision, more commonly known as a “Slow Mohs Surgery.” This involves removing the melanoma and delaying the stitching for a day or two in order to confirm clear margins.
While it would be ideal to process the tissue in-house at the time of the procedure (as is done in Mohs surgery), the melanoma cells can get distorted and harder to read when processed rapidly by freezing. Instead, the tissue is sent to an outside lab to be set in wax after processing in a formalin fixative. This allows the lab to obtain the highest degree of clarity of the pigment cells under the microscope. This “slow Mohs” or staged excision procedure offers margin control similar to Mohs surgery – a cure rate over 99% – and tissue sparing for melanoma removal.
Going forward, it is important to limit skin exposure to the sun’s harmful rays by wearing sunglasses, broad-brimmed hats, and protective, tightly woven clothing. Furthermore, use a broad-spectrum sunscreen rated at least SPF 30 or higher on all exposed skin, including the lips, even on cloudy days. Reapply sunscreen every 2 hours. Avoid tanning salons.
Monthly self-skin examinations and routine visits to your dermatologist are important for monitoring. Detecting melanoma early can be life-saving, since this cancer is very curable in the early stages. People with dark-complexions can also develop melanoma, especially on the palms of the hands, soles of the feet under nails and in the mouth. Therefore, these areas of the skin should be examined closely on a regular basis.
SCHEDULE A SKIN CHECK
Dr. Aradhna Saxena is a board-certified dermatologist and fellowship-trained Mohs surgeon specializing in screening and treating patients for all types of skin cancer. Melanomas typically present the most danger, but if they are detected and removed early enough, they can be eradicated. If you’ve seen any changes in your moles or other abnormal or new skin lesions, we urge you to schedule an appointment at the Dermatology and Skin Cancer Institute right away. We have offices in Fort Washington and Lansdale, PA.